Recommendations by ADA
In 2017, American Diabetes Association (ADA), published their updated Standards of Medical Care in Diabetes. Their recommendations include screening, diagnostic, and therapeutic actions that are known or believed to favorably affect health outcomes of patients with diabetes.
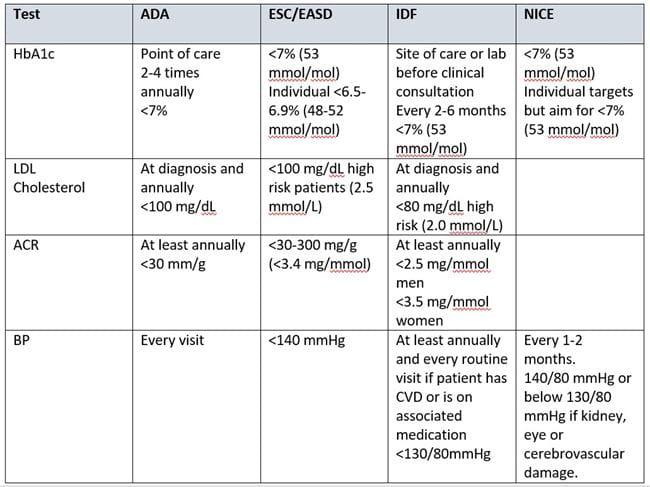
In the updated Standards of Medical Care, ADA included a section describing how often certain tests should be done and what goals a patient should achieve. All patients diagnosed with diabetes should regularly receive a comprehensive diabetes evaluation to determine the stability of their disease, response to medications, and evaluate any associated complications. For a full description see Standards of Medical Care in Diabetes – 2017.
ADA recommends HbA1c POCT whenever possible
A key test which should be performed at least 2-3 times a year is hemoglobin A1c (HbA1c). In adult patients who are not meeting glycemic goals or who have recently changed medications, the tests should be done quarterly. The ADA also recommends that providers utilize POCT for HbA1c to provide an opportunity for more timely treatment changes.
ADA added additional recommendations that an A1c testing without interference from hemoglobin variants should be used, as hemoglobin variants, assay interference, age, race/ethnicity, and conditions associated with red blood cell turnover would raise possibility of miscordance testing results between A1c testing and plasma glucose level.
In addition to HbA1c levels, an albumin:creatinine ratio (ACR) should be done more than once per year, including at least 3 tests in 6 months for confirmation after diagnosis and additionally after changes in medications.
Fasting lipid panels including LDL should be done at diagnosis, additionally to monitor therapy adherence, and annually along with liver function tests. Other tests at time of diagnosis should include serum creatinine and glomerular filtration rates. The ADA also recommends that blood pressure (BP) be evaluated at every routine visit.
Recommendations by ESC/EASD
The European Society of Cardiology (ESC) and European Association for the Study of Diabetes (EASD) joined forces to collaborate to generate guidelines on the management of diabetes mellitus, pre-diabetes and cardiovascular disease (CVD). Their guideline is written for the management of the combination of CVD and diabetes mellitus and not as a separate guideline for each condition. ESC/EASD note that consensus indicates that HbA1c of <7% should be targeted but with acknowledgment of the need to pay attention to the individual requirements of the patient.
Recommendations by IDF
In their comprehensive Global Guideline for Type 2 Diabetes, The International Diabetes Federation (IDF) recommend monitoring of blood glucose control by measurement of HbA1c. They recommend using high-precision methods standardized to criteria aligned to the international reference values and subject to stringent quality assurance testing.
Testing frequency is every 2 to 6 months depending on level, stability of blood glucose control and changes in therapy. The level recommended maintaining to minimize risk of developing complications is below 7% (53 mmol/mol). Lower HbA1c target may be considered if it is easily and safely achieved.
Blood pressure should be measured at least annually and at every routine clinic visit in people with know CVD. The recommended level is 130/80 mm Hg.
Kidney function should be assessed at diagnosis and annually by urine test for albuminuria and measurement of serum creatinine and calculation of eGFR.
Recommendations by NICE
In the updated guideline from 2017 with recommendations for managing diabetes type 2 in adults, NICE focuses on patient education, dietary advice, managing cardiovascular risk, managing blood glucose levels and identifying and managing long-term complications.
NICE recommends usage of methods to measure HbA1c that have been calibrated according to the International Federation of Clinical Chemistry (IFCC) standardization. As for HbA1c levels, the patient should be encouraged to achieve their individual target and maintain it unless any resulting adverse effects (including hypoglycaemia), or their efforts to achieve the target, impair their quality of life. If the levels rise to 7.5% 858 mmol/mol) or higher, they should aim for an HbA1c level of 7% (53 mmol/mol).
For blood glucose management, HbA1c levels should be measured at 3-6 months intervals (tailored to individual needs), until the HbA1c is stable on unchanging therapy and 6-montly intervals once the HbA1c level and blood glucose lowering therapy are stable.
NICE also recommend blood pressure to below 140/80 mmHg or below 130/80 mmHg if there is kidney, eye or cerebrovascular damage. Blood pressure should be monitored every 1-2 months.
Boronate Affinity
Boronate affinity assay for determination of the percentage of HbA1c in whole blood.
Standardization of the HbA1c measurement
Measuring accuracy - NGSP
There are strict regulations and controls for manufacturers of point-of-care systems. The products must fulfil certain standards, e.g. evaluation of performance and comparison with reference standards such as the National Glycohemoglobin Standardization Program (NGSP).
These requirements regarding measurement performance have become tighter. According to the latest NGSP for manufacturer certification, 37 out of 40 results should be within +/- 6%. For optimal clinical monitoring, an imprecision of 2% CV is desirable. This criterion is however very strict, and currently an imprecision of 3% CV is considered a more realistic goal.

