Recently, IDF analyzed similarities and discrepancies among currently available guideline in order to provide primary care physicians, hospital based clinicians and general practitioners with clinical practice recommendations to facilitate their daily decision-making process.
One of the cornerstones in the diagnosis, screening and treatment of diabetes is the measurement of blood glucose. It is the most commonly performed test at the point of care with HbA1c becoming more frequent.
Screening for T2D
Considering that up to 50% of people with T2D remain undiagnosed and untreated, and therefore more at risk for developing complications, most guidelines recommend screening for T2D in people above 40-45 of age and/or with high risk factors such as family history of diabetes, excess weight (obesity), abdominal obesity (increased waist circumference) and hypertension.
IDF recommends in their guideline, the use of a locally validated screening test such as the FINDRISC score. If this is unavailable, then a fasting blood glucose is recommended as screening test. The FINDRISC screening tool is available online and for download on www. idf.org.
The fasting blood glucose test is the most widely used test. Fasting blood glucose identify people with undiagnosed T2D and also people with intermediate hyperglycemia (“pre-diabetes”) who should be offered advice on how to reduce their risk of progression to T2D, e.g by changes in lifestyle and structured program.
People with a positive screening test should proceed to a diagnostic test. If the result of the test is normal, they should be advised on healthy lifestyle changes and the diagnostic test should be repeated every year. When negative, it is recommended that the screening test should be repeated at least every three years.
Recommendations for prevention of T2D
IDF conclude that some guidelines include recommendations on the prevention of T2D and there is consensus on the need for a structured prevention program. They identify that prevention of T2D in people with intermediate hyperglycemia (“pre-diabetes”) should focus on lifestyle modifications aimed to achieve at least a 5% to 7% weight reduction and increased physical activity. When a prevention program is not available, the primary care professional should team with a trained educator and develop a structured prevention program.
Diagnostic procedure
Most of the guidelines evaluated use the standard diagnostic criteria proposed by IDF and WHO. For the diagnostic procedure, IDF recommends the use of these criteria.
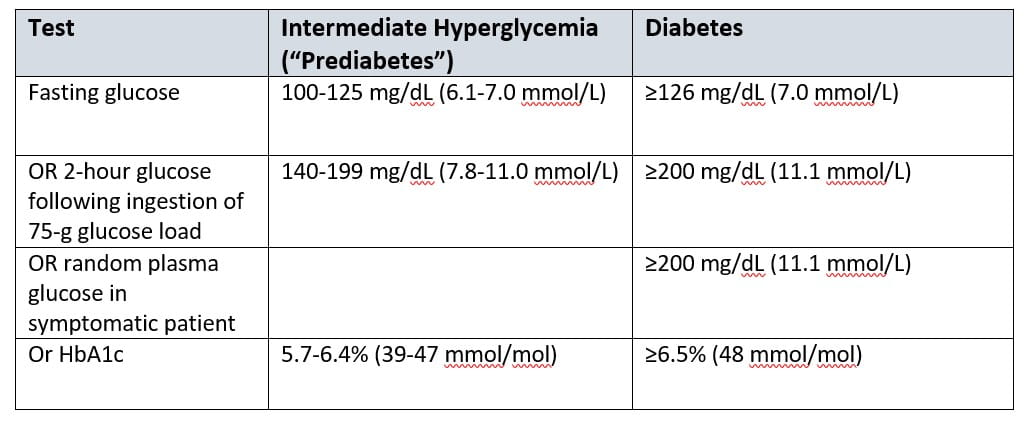
Furthermore, they acknowledge the use of HbA1c as a diagnostic test, particularly in those who are very likely to have the disease, since it will also be necessary to decide treatment and monitor its effectiveness. HbA1c should be an option for diagnosis, provided the results of the HbA1c test are standardized to those of the Diabetes Control and Complications Trial (DCCT) and United Kingdom Prospective Diabetes Study (UKPDS), which have established direct associations between HbA1c levels and outcome risks in people with diabetes.
In their guideline, they also encourage the primary care physicians to ensure that there is a standardized HbA1c test available in every primary care clinic. When a person is asymptomatic and the result of the diagnostic test is close to the normal range, the diagnosis should be confirmed in a second test.
Targets for glucose control
In their analysis of general target for glucose control in T2D, IDF conclude that most guidelines consider HbA1c less than 7% (53 mmol/mol) as the general target for glucose control. However, some consider that HbA1c should be <6.5% (48 mmol/mol). As long as hypoglycemia and weight gain can be avoided using appropriate treatments, lower HbA1c targets are desirable or at least should be considered. Values of HbA1c above 8% (64 mmol/mol) are generally unacceptable by all guidelines and blood glucose below 3 mmol/moL (54 mg/dL) should always be avoided.
Targets for glucose control in special populations
In patients using multiple medications including glucose-lowering drugs (GLDs) where predicted survival is short (eg. <10 years), with cognitive impairment, advanced chronic kidney disease (CKD) and severe cardio vascular disease (CVD) associated with multiple comorbidities, an HbA1c target between 7.5% and 8% (58 to 64 mmol/mol) may be more appropriate. Patients with those conditions should be referred to specialized care.
Monitoring glucose control
For glucose monitoring, the recommendation is that it should be mandatory for patients using insulin. IDF acknowledge glucose monitoring as useful not only during treatment adjustment but also during acute illness or as an education tool for self-care.
Other recommendations
Besides recommendations related to lifestyle changes, obesity, pharmacological treatment and add-on therapies, IDF also compared recommendations related to cardiovascular risk factors and other recommendations.
It is recognized by all guidelines that high blood pressure is a major risk factor for CVD and CKD. The diastolic blood pressure (DBP) should be 80 mmHg for people with T2D. However there is a discrepancy related to the systolic target, which varies between 140 and 130 mm Hg.
Another major cardiovascular risk factor is high blood lipid levels and particularly high LDL cholesterol.
Several guidelines include screening for microvascular complications in people with T2D from the time they are diagnosed and thereafter every 1 to 2 years.
Screening for nephorpahty includes measuring albumin excretion rate (AER) and glomerular filtration rate (GFR). The recommendation is to screen for albumin in urine every year. Treatment with and ACE inhibitor or an ARB is required for persistent albuminuria.
Serum creatinine should be measured every year to calculate eGFR once albuminuria is detected and/or when other risk factors are present (eg. hypertension).

